Thursday, February 23, 2006
Addin just bookmarks just for further reading
Tonight I read across some good links for further readings:
PSP fanboy
X'S Drive MP3 VP3650
Digital photography weblog
PDAnewsclip
Blogger use by furl
Engadget chinese
Writing weblog is just a beginning but maintainence is a great job.
However, you can ask bloggers from all around the world by internet and visiting other bloggers' websites. Knowlege is not only reading from books but from internet also. I need to work hard in order to manage my blog news in the further.
PSP fanboy
X'S Drive MP3 VP3650
Digital photography weblog
PDAnewsclip
Blogger use by furl
Engadget chinese
Writing weblog is just a beginning but maintainence is a great job.
However, you can ask bloggers from all around the world by internet and visiting other bloggers' websites. Knowlege is not only reading from books but from internet also. I need to work hard in order to manage my blog news in the further.
Hong Kong Tea Restaurant


Recently I read a newspaper introducing HK style tea restaurant in local Taipei city.
Anyone who is interested may go to try- cheap and delicious.
Sunday, February 19, 2006
Does diagnosis acute appenditicis affect by decreased WBC count?


A 49 y/o male patient came to ER due to severe epigastric pain shift to RLQ pain. WBC 19400 seg 92. We consulted GS and said appendicitis is not likely at present moment due to no rebound pain and suggest followup WBC +DC 6hrs later. Followup WBC+DC showed 13500 Seg 67 CRP 3.9 and patient felt better and felt some hungry. What will you do? Let him try feeding and discharge him or tell him appendicitis is not likely due to WBC count decreased?
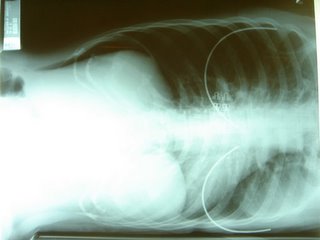
I check the patient who looks rather fat and obese abdomen. PE showed tenderness over Mcburny's point on deep palpation but marked rebound pain due to obesity. Bedside echo didn't showed any target sign but there is local tenderness during ultrasound examination. Abd CT showed enlarged appendix with wall thickening and perifocal fatty stranding(illustrated above). Operation showed engorged appendix with no perforation.
Discussion:
1. Acute appendicitis is diagnosed by clinically but not by laboratory data.
2. Followup WBC count if decreased does not mean decreased possibility of appendicits.
3. Don't rely too much on lab data or imaging, just rely on your basic physical examination.
Saturday, February 18, 2006
Bedside ultrasound use in diagnosis of PPU.



A 42 y/o female patient c/o sudden onset of epigastric pain since last night. PE showed marked epigastric tenderness but no rebound pain. BS is hypoactive. One of our resident check the patient and order a plain abd view and showed much stools but no free air. Primperan IV and eva enema is given by order. When I performed the bedside ultrasound, I found a lot of interruption echoic lying over right liver. I turn the patient to left decubitus view and showed free air in subphrenic area. Of course, my favorite X ray for diagnosis PPU-- chest left decubitus view first followed by standing CXR and standing plain abd. Since the patient cannot stand up for x ray examination(a hint for diagnosis of PPU), we take only the first 2 x rays and that are sufficient for diagnosis and finally call the surgeon for emergent operation. Operation findings showed PPU of course.
My ultrasound experience: Left decubitus position perform ultrasound>> If free air seen>> Go for X ray for chest left decubitus view>> standing CXR and standing plain abd.
Monday, February 13, 2006
X ray choice for diagnosis of PPU




Recently one of our resident order a KUB for a 62F with epigastric pain which LMD diagnosed GB stone. His first impression is acute cholecystitis. After I visit the patient, PE showed severe epigastric pain with decreased bowel sound, muscle guarding and rebound pain. ED echo showed much air reflections in supine view but when I turned the patient to left decubitus view, there are several air reflections over right liver dome and without movements during respiration >> free air. Then I sent the patient for a chest left decubitus view and then a sitting Chest PA view. Finally the X rays showed much free air under right diaphragm which later prove to be PPU.
Epigastric pain + free air in left decubitus view by echo>> 100% subphrenic free air will be shown in either or both left decubitus view and/or sitting/standing Chest PA.
Suggestions:
1. For abd pain above the umbilicus>> order plain abdomen.
2. For abd pain below the umbilicus>> order KUB.
3. Abdominal ultrasound is the choice of examination in acute abdomen besides traditional X rays.
4. If the above measures didn't showed any free air, then an CT scan without contrast is needed to show the subphrenic free air.
MOZART ON THE ROAD


Recent I pay a visit to TWTC for Taipei International Books Exhibition. There are a lot of new books, magazines and foreign books. I got not much time to read in detail since I had to work at night. But I do buy a book about Mozart with 4 CDs which is an 250 yrs anniversity of this great composer in history.
3rd Asian Pacific Congress of Heart Failure 2006
3rd Asian Pacific Congress of Heart Failure will be held in TICC from Oct. 27-30, 2006.
Check in the website here and make sure the abstract deadline before June , 30, 2006.
Registration Free
Categories >>Free
Early registration(before August 31,2006)>>US$ 250
On-site registration(after August 31,2006)>>US$ 350
Trainee/Student>>US$ 150
Daily registration>>US$ 180
Accompanying person>>US$ 150
TSCCM Members 重症醫學會會員>>Free ***
Check in the website here and make sure the abstract deadline before June , 30, 2006.
Registration Free
Categories >>Free
Early registration(before August 31,2006)>>US$ 250
On-site registration(after August 31,2006)>>US$ 350
Trainee/Student>>US$ 150
Daily registration>>US$ 180
Accompanying person>>US$ 150
TSCCM Members 重症醫學會會員>>Free ***
Saturday, February 11, 2006
Primperan + Ketorolac
Recently I encountered a case of 22 female patient c/o abd pain came to ED 3 days ago and discharged. The patient came back again due to persisted abd pain and later fever up to 39.3C.
2/3 2043 c/o epigastric pain BT 37.6C WBC 16500 Seg 87 B1
Primperan + Keto (resident routine treatment for abd pain)
MBD but still complained of abd cramping pain. WBC 9800 Seg 79 B2
Primperan + Keto (resident routine treatment again) then MBD.
2/6 0702 c/o lower abd pain with rebound pain WBC 17600 Seg 81 CRP 12.2
Transfer to fever ward due to fever 38.6 C>>39.3C
Abd CT report--
CT scan of whole abdomen with and without contrast enhancement:1. A tortuous tubular structure with wall thickening and increased enhancement in right pelvic cavity may be due to dilated fallobian tube. Fat stranding in the pelvic cavity as well as fluid accumulation are also noted, suggesting PID with possible pyosalpinx.(Radiologist said appendicitis is not likely by imaging)
Consult GYN- RLQ pain R/O acute appendicitis
Consult GS- Clinically acute appendicitis is not likely at present.
GYN prepare for lapraoscope- appendicitis rupture with ascites>> Consult GS to take over>> retrocecal appendicitis with rupture.
Discussion:
1. Is primperan + Keto a routine treatment protocol for abd pain by resident, even senior resident?
2. After the first NSAID given, is it necessary to survey the patient before one order the second NSAID injection?
2/3 2043 c/o epigastric pain BT 37.6C WBC 16500 Seg 87 B1
Primperan + Keto (resident routine treatment for abd pain)
MBD but still complained of abd cramping pain. WBC 9800 Seg 79 B2
Primperan + Keto (resident routine treatment again) then MBD.
2/6 0702 c/o lower abd pain with rebound pain WBC 17600 Seg 81 CRP 12.2
Transfer to fever ward due to fever 38.6 C>>39.3C
Abd CT report--
CT scan of whole abdomen with and without contrast enhancement:1. A tortuous tubular structure with wall thickening and increased enhancement in right pelvic cavity may be due to dilated fallobian tube. Fat stranding in the pelvic cavity as well as fluid accumulation are also noted, suggesting PID with possible pyosalpinx.(Radiologist said appendicitis is not likely by imaging)
Consult GYN- RLQ pain R/O acute appendicitis
Consult GS- Clinically acute appendicitis is not likely at present.
GYN prepare for lapraoscope- appendicitis rupture with ascites>> Consult GS to take over>> retrocecal appendicitis with rupture.
Discussion:
1. Is primperan + Keto a routine treatment protocol for abd pain by resident, even senior resident?
2. After the first NSAID given, is it necessary to survey the patient before one order the second NSAID injection?
Thursday, February 09, 2006
14th Congress of Asia-Pacific Association of Critical Care Medicine (APACCM 2006)
The 14th Congress of Asia and Pacific Association of Critical Care Medicine (APACCM2006) will be held from Aug. 26 to 29, 2006 in Beijing, China.
Check the website here and remember the abstract submission on line is started now and deadline: April , 10, 2006.
Check the website here and remember the abstract submission on line is started now and deadline: April , 10, 2006.